Peptides & Tissue Remodeling for Injured Athletes
Executive Summary
For athletes, injury recovery isn’t just about closing a wound or waiting until pain subsides—it’s about remodeling tissue so it can handle sport-level loads again. Poorly remodeled tissue often means more scar tissue, weaker collagen, and higher re-injury risk. Peptides such as BPC-157, Thymosin β4, and GHK-Cu show promise in supporting remodeling by guiding collagen organization, improving angiogenesis, and balancing enzymes that break down or build tissue.
Key points for athletes:
- What remodeling is: the transformation from a temporary patch to durable, sport-ready tissue.
- Why it matters: scars and disorganized collagen make reinjury more likely.
- Peptides’ role: accelerate organization, improve vascularity, and reduce adhesions.
- Practical benefits: potentially shorten return-to-sport timelines by 1–3 weeks within an overall healing window of 3–8 weeks for muscle strains and 6–16+ weeks for ligament injuries (based on animal and human-adjacent evidence).
- Age & health factors: older or metabolically challenged athletes may see greater benefits due to slower natural remodeling.
- Surgery: peptides may help reduce adhesions and improve tendon-bone integration after procedures like rotator cuff or ACL repair
What is Tissue Remodeling?
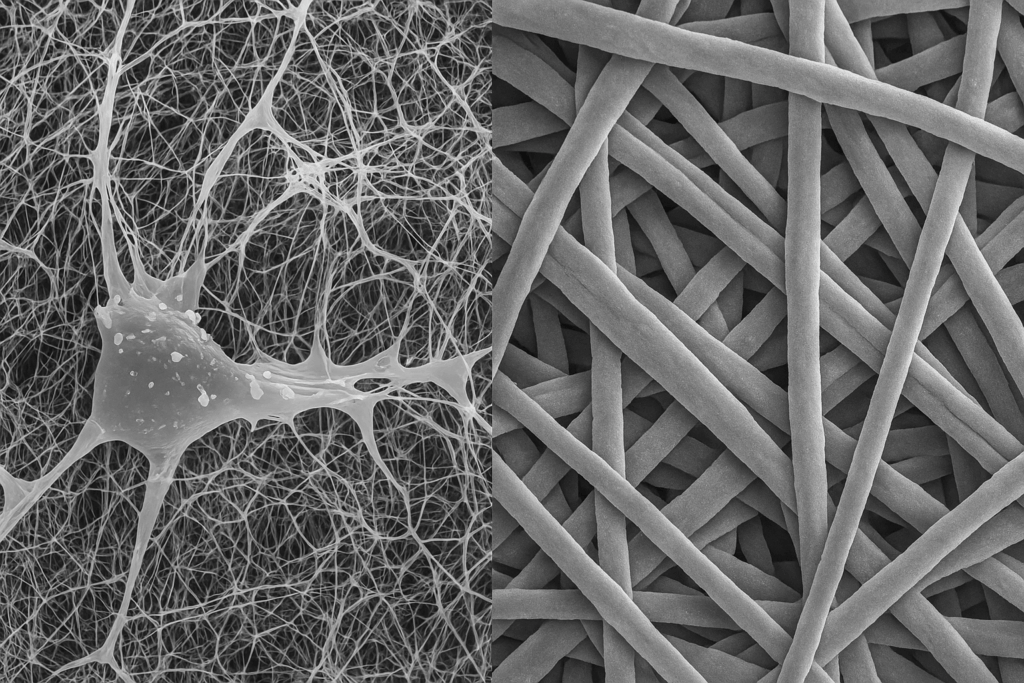
Remodeling is the late stage of healing where the body reorganizes collagen and extracellular matrix. In simple terms: early healing builds a patch (fibrin clot → type III collagen), remodeling shapes that patch into a performance-ready structure (type I collagen). Collagen fibers realign, cross-links mature, vascularity normalizes, and scar tissue gradually becomes stronger and more elastic.
Why Improper Remodeling Increases Reinjury
Disorganized, scar-heavy tissue is biomechanically inferior—weaker, less elastic, and poorly aligned with sport-specific load. Tendon proteomics shows some fibers have half-lives of hundreds to thousands of days, meaning once poor-quality scar is laid down (dominated by type III collagen), it may persist for years. This is why athletes with prior injuries often struggle with repeat tears.
Scar Tissue: Formation, Breakdown, and Remodeling
- Formation (days 0–7): fibroblasts deposit type III collagen (thin, quick “patch” fibers) in a chaotic pattern; vascular sprouting occurs, anchored initially by a fibrin clot.
- Early remodeling (weeks 1–6): enzymes (MMPs) break down misaligned type III collagen, and new collagen starts to realign.
- Late remodeling (6 weeks–12+ months): type I collagen (thicker, stronger, sport-ready fibers) replaces type III, tensile strength improves, and vascularity normalizes.
For athletes, this means the real danger zone isn’t just the first week—it’s the months when remodeling determines long-term strength.
Why Peptides May Be the Difference Between Full Healing and Chronic Injury
Many athletes — especially those over 40 — know the frustration of an injury that never quite feels the same again. The science supports this:
- Incomplete remodeling is common. Studies show that even after 12 months, many tendons and ligaments retain excess type III collagen and disorganized fiber orientation (1,2).
- Recovery capacity declines with age. Older athletes have slower angiogenesis, reduced fibroblast activity, and stiffer collagen cross-links, leaving the tissue more likely to plateau in a “half-healed” state.
- Chronic injuries = incomplete remodeling. Tendinopathy, stubborn hamstring pulls, and post-surgical adhesions often trace back to inadequate remodeling rather than the initial tear itself.
Where peptides fit:
- BPC-157 and Thymosin β4 may boost angiogenesis and fibroblast migration, preventing the stalled healing seen in older athletes.
- GHK-Cu helps remodel established scar by balancing MMP/TIMP activity, giving a “second chance” at reorganizing poorly healed tissue.
- In effect, peptides may bridge the gap between the body’s limited recovery capacity and the demands of sport, making the difference between a return to full performance or sliding into chronic injury.
For older athletes, this can mean the difference between finishing a season strong versus living with recurring pain or instability.
Peptides for Tissue Remodeling
BPC-157
- Mechanism: stimulates angiogenesis, fibroblast migration, nitric oxide pathways.
- Evidence: rat models show accelerated tendon fibroblast outgrowth and better collagen organization (shift from disorganized type III collagen toward type I collagen) (3). Reviews highlight faster tendon and ligament recovery across models (4,5).
- Athlete angle: stronger, better-aligned collagen may reduce recurrence risk when load ramps up.
Thymosin β4 (TB-500 fragment)
- Mechanism: promotes angiogenesis, cell migration, and early ECM deposition.
- Evidence: animal and wound-healing models show faster closure, better vascularization, and improved repair quality (6).
- Athlete angle: most useful in the early weeks post-injury, when blood supply and cell migration set the stage for quality remodeling.
GHK-Cu
- Mechanism: upregulates collagen and elastin genes, improves MMP/TIMP balance, reduces oxidative stress.
- Evidence: human studies (skin) show improved collagen density and elasticity in 8–12 weeks (7,8).
- Athlete angle: while best data is in skin, mechanisms suggest value for scars and adhesions, especially post-surgery or in chronic injuries.
Healing With vs. Without Peptides
| Approach | Remodeling Quality | Estimated Return-to-Sport (muscle/ligament) | Athlete Impact |
| Standard rehab only | Disorganized type III collagen gradually shifts toward type I collagen, but often incompletely | 3–8 weeks (muscle) / 6–16+ weeks (ligament) | Higher chance of stiffness, adhesions |
| Peptides from day 0 | Faster fibroblast migration, earlier type I collagen alignment | 2–6 weeks (muscle) / 5–12 weeks (ligament) | Potentially quicker, stronger return |
| Peptides after “healed” | Breakdown of disordered type III collagen and stimulation of type I remodeling | 4–12+ weeks functional gains | Useful for chronic stiffness, adhesions |
Numbers are conceptual estimates; based on animal/human-adjacent evidence, not guaranteed outcomes.
Age, Health, and Recovery Capacity
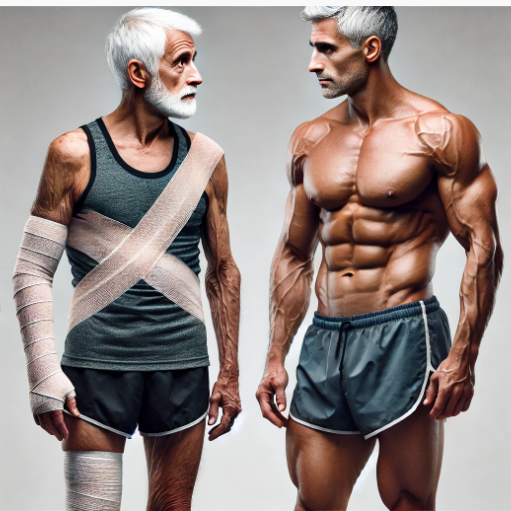
- Younger athletes: faster baseline remodeling (fibrin clot → type III collagen → type I collagen progression is efficient); peptides may shorten time but gains are modest.
- Masters athletes (40–60+): slower collagen turnover, weaker angiogenesis, and stiffer scars; peptides may provide proportionally larger benefits (1,2).
- Metabolic health matters: insulin resistance, low protein intake, or sleep debt all slow remodeling, regardless of peptide use.
Surgical Repair Applications
In post-op athletes (rotator cuff, ACL, Achilles):
- Early phase (0–6 weeks): BPC-157 and TB-4 may improve angiogenesis and ECM deposition, supporting tendon-bone integration and transition from fibrin clot to organized collagen (3–6).
- Remodeling phase (6–16 weeks): GHK-Cu may improve scar quality and accelerate the type III → type I collagen shift, especially when paired with progressive rehab (7,8).
- Late phase: peptides may help reduce adhesions and stiffness, supporting a more functional return.
Key Takeaways for Athletes
- Remodeling determines future durability of your injured tissue.
- Many chronic injuries stem from incomplete remodeling rather than the initial tear.
- Peptides like BPC-157, Thymosin β4, and GHK-Cu may improve scar quality, collagen alignment, and full recovery potential.
- Benefits appear greater in older athletes, where peptides may be the difference between fully healed and chronic nagging injury.
- For best results, biology must be paired with structured loading, nutrition, and recovery discipline.
References
- Heinemeier KM, et al. Lack of tissue renewal in human adult Achilles tendon. FASEB J. 2013;27(5):2074-2079.
- Choi H, et al. Half-lives of protein turnover in human tendon proteome. Sci Transl Med. 2020;12(574):eaay4361.
- Chang CH, et al. BPC-157 promotes tendon fibroblast outgrowth and healing in rats. J Orthop Res. 2011;29(6):976-983.
- Staršinić M, et al. Review: BPC-157 and musculoskeletal healing. Curr Pharm Des. 2020;26(25):2865-2874.
- Japjec M, et al. BPC-157 in tendon, ligament, and muscle healing. Biomedicines. 2021;9(9):1257.
- Su L, et al. Thymosin β4 and tissue repair: mechanisms and applications. Front Pharmacol. 2018;9:428.
- Pickart L, et al. GHK-Cu peptide regulates gene expression related to ECM remodeling. J Biomater Sci Polym Ed. 2012;23(8):1051-1073.
- Maquart FX, et al. GHK-Cu stimulates collagen synthesis in human fibroblasts. FEBS Lett. 1988;238(2):343-346.