The “Spark” in the Brain: Why Women Are Turning to PT-141
For many women, low libido is not a failure of hormones or physical capability—it is a breakdown in neurological signaling. Desire often fades not because the body is incapable, but because the brain is overloaded, distracted, or locked into chronic stress patterns. PT-141 (Bremelanotide) represents a fundamentally different approach to female sexual wellness by acting directly on the central nervous system, restoring the mental spark that initiates arousal. Rather than forcing a response, PT-141 appears to help reconnect the brain and body—allowing desire, sensitivity, and spontaneity to re-emerge naturally.1-3

The “Spark” in the Brain
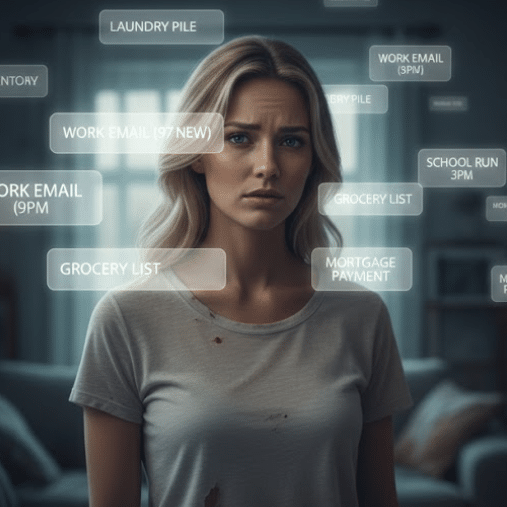
For many women, the challenge of low libido isn’t a physical one; it’s a connection one. You may have balanced hormones, a partner you love, and a healthy body—yet the mental pilot light has gone out. This is especially common for women navigating chronic stress, long-term relationships, perimenopause, or the cognitive overload of modern life, where desire doesn’t disappear—it simply goes quiet.4
This is where PT-141 (Bremelanotide) is changing the conversation around female sexual wellness.
Unlike traditional approaches that focus on hormones or local creams, PT-141 targets the central nervous system. It doesn’t just prepare the body; it invites the mind back into the room.1
The Brain–Body Connection: How It Works
Scientific literature describes female arousal as an “upstream” process. If the brain does not initiate the signal, the body often fails to respond—regardless of hormone levels or physical readiness.5
PT-141 works by activating melanocortin receptors, particularly melanocortin-4 receptors (MC4R), which play a role in desire, motivation, and reward signaling. These neural pathways are distinct from those involved in hormonal regulation or genital blood flow, helping explain why PT-141 produces effects that feel cognitive and emotional rather than purely physical.1-3
The Ignition Switch
Think of PT-141 as an ignition switch. While hormones such as estrogen and testosterone provide the fuel, PT-141 supplies the spark that actually starts the engine.
Lowering the “Noise”
For many women, stress and constant mental chatter act as a brake on desire. PT-141 appears to help bypass these mental blocks, lowering the threshold required to feel genuine, spontaneous arousal. Many women describe it as the difference between wanting intimacy while feeling mentally scattered—like having dozens of browser tabs open—and suddenly having that internal noise go quiet.4-6
Non-Hormonal
Because PT-141 is a peptide and not a hormone, it offers an option for women who cannot—or simply choose not to—use Hormone Replacement Therapy (HRT).1
Beyond the Diagnosis: What Women Report
While PT-141 is clinically approved for Hypoactive Sexual Desire Disorder (HSDD), observational feedback shared across wellness communities and long-form health podcasts suggests that its perceived benefits often extend beyond a single diagnosis.1-2
Reclaiming Spontaneity
The most commonly reported experience is the return of spontaneous thought. Instead of intimacy feeling like a chore or a scheduled “to-do,” many women describe the reappearance of unprompted thoughts of closeness and desire—the kind that may have been missing for years.
Enhanced Orgasm and Sensitivity
Across forums and biohacking podcasts, women frequently describe what they experience as a noticeable “sensory upgrade.”
Many report orgasms that feel deeper, longer, and easier to reach. Others describe physical touch as more “electric,” allowing foreplay to feel immersive and natural rather than mechanical or goal-oriented.2-3
Reducing the “Desire Gap”
Low libido often creates a cycle of guilt, pressure, and relationship strain. PT-141 is frequently discussed as a tool that helps women step out of their heads and reconnect with their partners—without the burden of forced performance or expectation.4
Protocol & Comfort: The “Gentle Start”
For women, the standard clinical dose (1.75 mg) can be unnecessarily strong, with nausea being the most common side effect.1 In practitioner-guided wellness settings, many women begin with a Gentle Start Protocol.
Because PT-141 acts centrally rather than locally, significantly lower doses often produce the desired cognitive-emotional effect.3
Many women start in the 0.5 mg to 0.75 mg range to assess sensitivity. This low-and-slow approach is commonly reported to deliver the mental spark while avoiding stomach discomfort.1-2
Timing and Frequency
Most practitioners recommend no more than 2–3 uses per week, with at least 48 hours between doses.
In practical terms, this typically translates to no more than 6–8 uses per month, with many clinicians preferring to remain at the lower end of that range for ongoing use. PT-141 is not intended for daily or continuous use.
Why There’s a Monthly Cap (Not Just Weekly)
The monthly limit is not arbitrary—it is driven by central nervous system biology, not toxicity.
Melanocortin receptor desensitization: PT-141 activates MC4 receptors involved in motivation and reward. Repeated overstimulation without sufficient recovery time can blunt responsiveness, leading to a diminished effect over time and, in some cases, a perceived need for higher doses to achieve the same response.2-3
Preserving spontaneity: Ironically, overuse may make desire feel less spontaneous by turning PT-141 into a crutch rather than a signal-restoring tool. Intermittent use helps preserve the brain’s natural ability to respond.
Side-effect creep: Nausea, flushing, or headache may be minimal early on but can become more noticeable with frequent or clustered use.1
Alignment with clinical safety data: Even though wellness protocols often use lower doses, staying within a similar monthly exposure window as studied clinical protocols is generally considered prudent.1-2
How Many Women Actually Use It (Real-World Pattern)

In practice, many women settle into one of the following patterns:
“Reconnect” phase: Used 1–2 times per week for a few weeks (approximately 4–6 uses per month) to help re-establish desire signaling.
Maintenance or situational use: Used 2–4 times per month, often aligned with relationship rhythms, travel, or periods of intentional connection.
Occasional use: Used on an as-needed basis, well below monthly caps, once confidence in responsiveness has returned.
Pro Tips for a Better Experience
Within wellness communities, several practical strategies are frequently shared to improve comfort and consistency. Individual sensitivity varies, and these approaches are most often discussed in practitioner-guided contexts.
Ginger support: Ginger has demonstrated antiemetic effects and is commonly used to reduce peptide-associated nausea.7
Hydration and electrolytes: Adequate hydration may help reduce mild flushing or facial warmth that can occur shortly after use.1
Antihistamine support: Some practitioners suggest a non-drowsy antihistamine (such as loratadine) to blunt histamine-mediated effects like congestion or nausea.8
Conclusion
PT-141 is not about forcing desire—it is about restoring the neurological signal that allows desire to emerge naturally. For women who feel disconnected from their sexuality despite having “everything else in place,” this peptide represents a brain-first approach to intimacy.
Rather than manufacturing arousal, PT-141 appears to help quiet mental interference, re-engage motivational pathways, and allow desire, sensitivity, and pleasure to return as something familiar—not artificial. When used thoughtfully and intermittently, it offers a way to reconnect with intimacy without altering hormones or overriding the body’s natural rhythms.
References
- Kingsberg SA, Clayton AH, Portman DJ, et al. Bremelanotide for the treatment of hypoactive sexual desire disorder in premenopausal women. Obstet Gynecol. 2019;134(5):899-908.
- Clayton AH, Kingsberg SA, Goldfischer ER, et al. Evaluation of the safety and efficacy of bremelanotide in women with HSDD. J Sex Med. 2016;13(11):1684-1696.
- Pfaus JG, Kippin TE, Centeno S. Melanocortin signaling and sexual motivation. Neurosci Biobehav Rev. 2018;86:24-34.
- Brotto LA, Basson R. The impact of stress and cognition on female sexual desire. J Sex Res. 2014;51(2):101-116.
- Basson R. The female sexual response: A different model. J Sex Marital Ther. 2000;26(1):51-65.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374-381.
- Lete I, Allué J. The effectiveness of ginger in the prevention of nausea and vomiting. Integr Med Insights. 2016;11:11-17.
- Simons FER, Simons KJ. Histamine and H1-antihistamines. N Engl J Med. 1994;330(23):1663-1670.
- Hadley ME, Haskell-Luevano C. The proopiomelanocortin system. Endocr Rev. 1999;20(3):202-230.
- Thaler RH, Macdonald PM. Central nervous system regulation of sexual motivation. Physiol Behav. 2017;176:139-148.